Cancer Diagnosis: Understanding the Process and What Comes Next
When dealing with cancer diagnosis, the systematic process of identifying cancer type, stage, and spread. Also known as cancer detection, it guides treatment plans and informs prognosis. A crucial companion to diagnosis is early detection, the practice of spotting cancer before symptoms appear, which often hinges on effective screening tests, medical exams or imaging used to find hidden disease. Together, these elements shape the odds of a favorable outcome.
Why does early detection matter? It directly reduces the time between disease onset and treatment, a factor linked to higher survival rates, statistics that measure how many patients live past a specific time after diagnosis. The semantic link is clear: cancer diagnosis encompasses early detection, and early detection requires reliable screening. Common screening tools—mammograms for breast cancer, colonoscopies for colorectal cancer, low‑dose CT scans for lung cancer—serve as the bridge between hidden disease and timely care.
The Symptom‑Screening Connection
Symptoms act as the body's alarm system, prompting doctors to order targeted screening tests. Persistent cough, unexplained weight loss, or a new lump are red flags that often lead to imaging or biopsy. This relationship forms a second semantic triple: symptoms guide the need for screening, and screening influences survival rates. Recognizing warning signs early can shorten the diagnostic pathway, giving patients a better chance at effective treatment.
Beyond the medical facts, the emotional side of a cancer diagnosis cannot be ignored. Knowing that early detection and proper screening improve survival can provide patients and families with a sense of control. It also helps healthcare providers prioritize resources, such as arranging rapid follow‑up appointments for high‑risk individuals.
From a practical standpoint, staying on top of recommended screening schedules is a simple yet powerful habit. For example, men over 50 should discuss PSA testing with their doctor, while women should schedule regular mammograms starting at age 40. These actions create a proactive loop: regular screening boosts early detection, which in turn lifts survival rates. This loop embodies the third semantic triple: early detection requires screening tests, and screening tests improve survival outcomes.
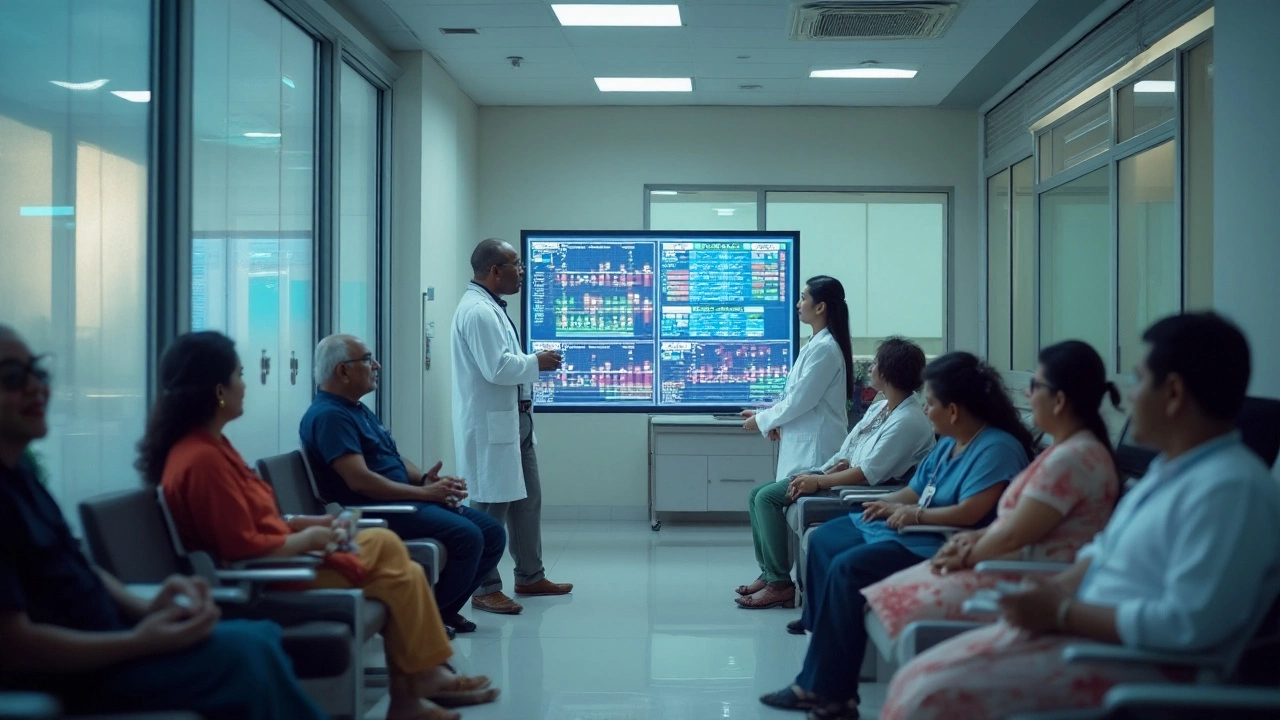
Technology is shifting the landscape of cancer diagnosis as well. AI‑driven image analysis, liquid biopsies, and genetic profiling are emerging tools that promise faster, more accurate detection. While still evolving, these innovations reinforce the core principle that better detection methods lead to earlier diagnosis and better survival chances.
Health policies also play a role. Government‑sponsored screening programs and insurance coverage for preventive tests remove financial barriers, making it easier for at‑risk populations to access early detection services. When access improves, population‑wide survival rates tend to rise—a fourth semantic connection linking policy, screening, and outcomes.
In short, a solid grasp of how cancer diagnosis interacts with early detection, screening, symptoms, and survival can empower you to take meaningful steps. Below, you’ll find a curated collection of articles that dive deeper into each of these topics, offering practical advice, recent research findings, and real‑world examples to help you navigate the journey ahead.